Microbiology - Staphylococcus Aureus and Skin Abscess
Short Summary:
This video explains the formation of skin abscesses, primarily caused by Staphylococcus aureus. It details the virulence factors of S. aureus, such as its capsule, adhesion proteins (fibronectin and collagen binding proteins), protein A (which inhibits antibody binding), and the enzymes coagulase (forms fibrin clots) and staphylokinase (breaks down fibrin clots). The video describes the immune response to S. aureus infection, including the roles of dendritic cells, macrophages, mast cells, and neutrophils. The process of abscess formation is explained as a result of the battle between the bacteria and the immune system, leading to the accumulation of pus (dead leukocytes, bacteria, and tissue debris) within a contained capsule. The video emphasizes the opportunistic nature of S. aureus, highlighting its ability to exploit skin breaches to cause infection.
Detailed Summary:
The video begins with an introduction to skin abscesses, defining them as localized infections characterized by neutrophil accumulation and tissue necrosis, mainly caused by Staphylococcus aureus. The speaker then focuses on the microbiology of S. aureus, describing it as a gram-positive coccus with circular DNA and plasmids (often containing resistance genes).
Next, the video details the virulence factors of S. aureus:
- Capsule: Resists phagocytosis.
- Adhesion proteins (fibronectin and collagen binding proteins): Allow the bacteria to attach to host cells.
- Protein A: Prevents antibody binding. The speaker uses a diagram to illustrate how Protein A binds to the Fc region of the antibody, preventing the Fab region from binding to the bacteria.
- Exotoxins (TSST-1 and enterotoxins): Briefly mentioned but not detailed.
- Invasins (coagulase and staphylokinase): Coagulase converts fibrinogen to fibrin, forming a protective clot around the bacteria. Staphylokinase breaks down fibrin clots, allowing the bacteria to spread. The speaker emphasizes the importance of understanding this dual mechanism of clot formation and degradation.
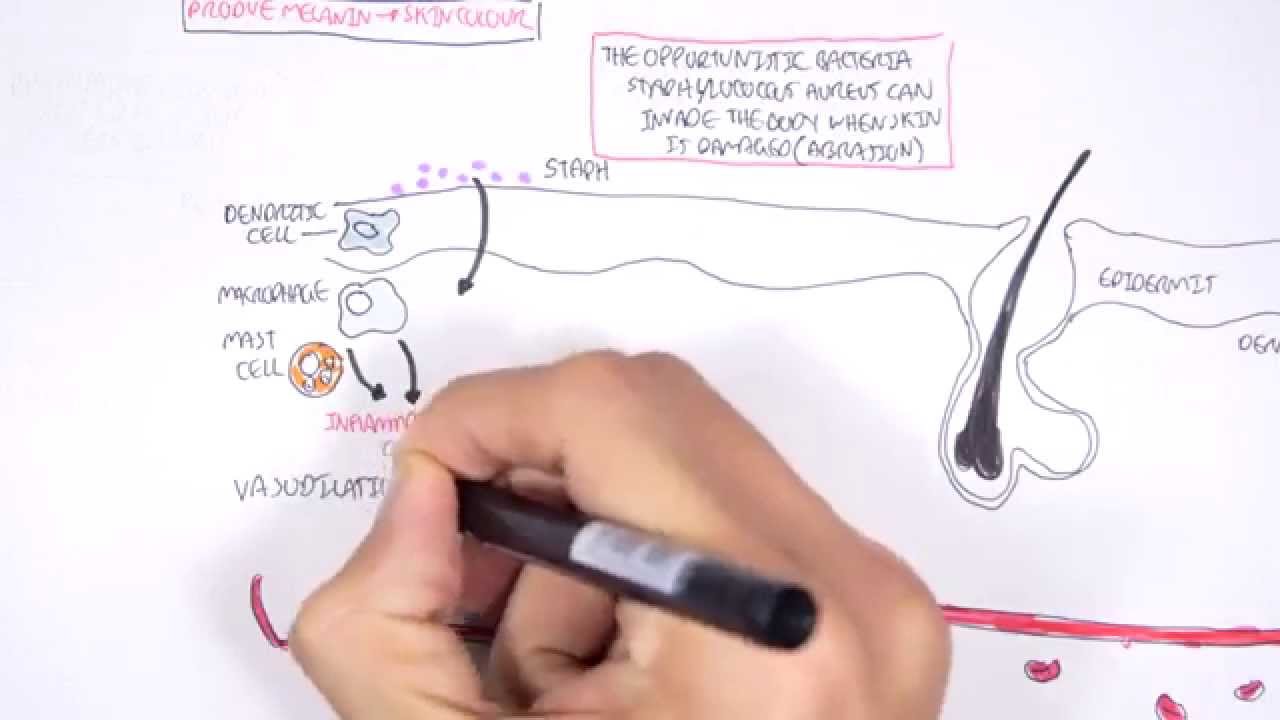
The video then shifts to the pathogenesis of abscess formation. Using a diagram of skin layers (epidermis and dermis), the speaker shows the location of immune cells like dendritic cells, macrophages, and mast cells. The process is described as follows:
- S. aureus, a commensal bacterium, enters the body through a skin breach (abrasion, burn, cut).
- Immune cells detect the bacteria and initiate an immune response, releasing inflammatory cytokines (TNF-alpha, interleukin-1, and histamine).
- Vasodilation and increased vascular permeability occur, recruiting neutrophils to the site of infection.
- Neutrophils attempt to phagocytose the bacteria, but many die in the process.
- The accumulation of dead neutrophils, bacteria, and tissue debris forms pus, creating the abscess.
- Fibroblasts contribute to the formation of a capsule around the abscess.
The video concludes by summarizing the process and emphasizing the role of S. aureus's virulence factors in protecting it from the immune system and facilitating abscess formation. No specific technologies are mentioned beyond the basic microbiological techniques used to study bacteria. The implications are the understanding of skin infection pathogenesis and the importance of proper wound care to prevent such infections.